African American Health Issues in the North: Discrimination and Poverty
Health issues that would plague generations of African Americans in northern cities in the twentieth century, including patients treated by the Philadelphia General Hospital in the three decades after the Second World War, can be traced to cities’ discriminatory health and employment policies and practices, which found support in the writings of anti-black race-writers.
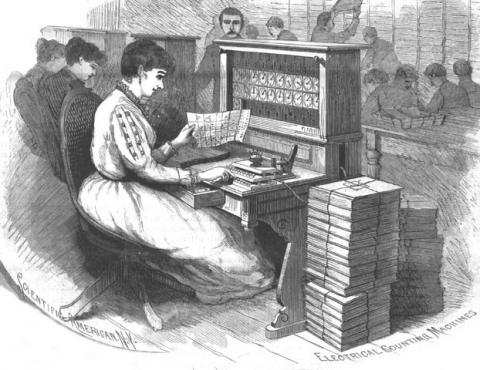
At the turn of the twentieth century, anti-black race-writers provided perverse justifications for denying essential social and health services to African Americans in segregated northern cities. Statisticians such as Frederick Hoffman interpreted indicators they found in the 1890 Census as conclusive evidence that African Americans were a diseased and dying population group—hence their recommendations to policy makers to deny essential social and health services to this population. Hoffman and others like him foisted their own racist assumptions onto their data and ignored social conditions born of racial isolation and discrimination that spawned the indicators they badly misinterpreted.
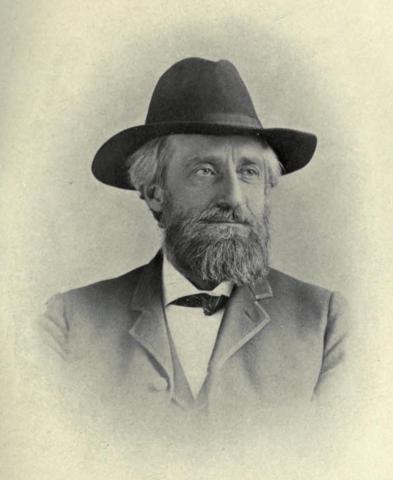
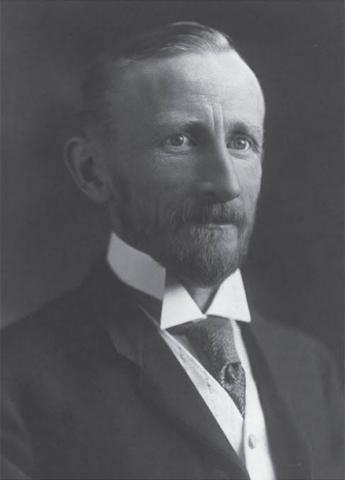
In a brilliant book The Condemnation of Blackness (2010), the social historian Khalil Gibran Muhammad looks closely at anti-black stereotypes advanced by white social scientists and thought-leaders in the urban North from 1890 to 1930. These anti-black social theorists portrayed African Americans as a degenerate race. The hostile doctrine of black inferiority they promoted paralleled—and gave a stamp of approval to—Jim Crow segregation and the violence perpetrated against blacks in the South. In the North, white social scientists justified their claims about black intelligence and morality on the basis of statistics that showed high levels of black disease, impoverishment, and criminality. That African American migrants from the South were forced to live as social outcasts in crowded segregated neighborhoods marked by dire poverty, job discrimination, and a dearth of social and health services—environmental conditions that were the hallmarks of social abandonment. No individual contributed more to the myth of black degeneracy and decline than Frederick L. Hoffman, chief statistician for the Prudential Insurance Company, whose book Race Traits and Tendencies of the American Negro was taken as gospel among Northern policy makers and white social reformers.[1]
The main line of Muhammad’s argument goes as follows: Northern white race-writers at the turn of the last century studied indicators in the 1890 Census which they (wrongly) interpreted to show a black tendency to disease and extinction (as reported by Hoffman: “a race proclivity to disease and death”). What they saw in the statistical indicators provided, to their minds, confirmation that Southern blacks born after 1865 and passage of the 13th Amendment had regressed to a primitive, pre-slavery-African state. In other words, absent the “civilizing” influence of plantation slavery, the black race was written off as doomed (at the time at least 90 percent of African Americans lived in the rural South). Why couldn’t blacks elevate themselves to the equal status of whites? asked race-writers like Frederick Hoffman, statistician for the Prudential Insurance Company. Blinded by their racism, they answered their own question: blacks were biologically, hence intellectually, inferior to whites; moral inferiority was an assumed byproduct of intellectual inferiority, with moral inferiority invoked to explain high rates of tuberculosis, alcoholism, prostitution and other markers of criminal behavior. Such was Hoffman’s hostility that he declared black Americans fatally prone to venereal disease without a whit of data to support the claim. Hoffman “asserted that ‘any physician who practiced among the colored people’ would attest that as many as 75 percent of them were ‘cursed’ with a sexually transmitted disease.” Such was the sorry state of the quantitative component of American social science at the turn of the last century.[2]
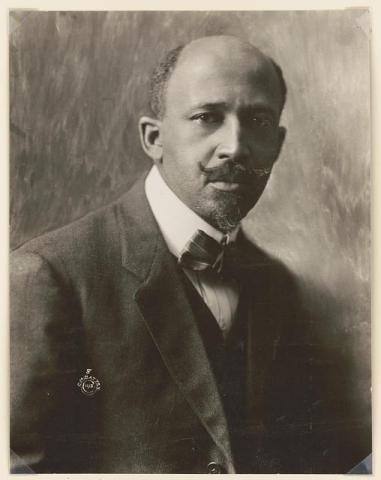
Hoffman and other white social scientists of his generation, with few exceptions, were predisposed by their engrained racism to dismiss racial discrimination as the key factor in the unhealthful environmental conditions and high levels of stress that prevailed in poor and working poor African American neighborhoods like Philadelphia’s 7th Ward, which W.E.B DuBois exhaustively reported on in The Philadelphia Negro, his comprehensive social survey of life and social conditions in this ward in South Philadelphia. Though sponsored and published by the University of Pennsylvania in 1899, The Philadelphia Negro attracted no critical acclaim and remained virtually unknown in scholarly circles for most of the next century.[3] Then things changed. As race relations continued to roil in urban centers in the aftermath of the Civil Rights Movement, black scholars in African American studies departments and programs began to take up DuBois’s banner, and The Philadelphia Negro achieved iconic status in the field.[4] The core problem of the so-called Negro Problem was not something inherently wrong with blacks, it was racial discrimination and the effects of poverty.
That white thought-leaders, policymakers, heads of social and health agencies, and social workers took the anti-black pronouncements of the bigoted race-writers to heart had dire real-world consequences for the residents of neighborhoods like the 7th Ward. Written off as morally deficient, prone to criminality, and diseased, they were denied essential social and health services, not to mention police protection. Yet these same services were available to European immigrants, whom reformers regarded as assimilable. It was of little practical benefit to urban blacks when, in the 1920s, social scientists shifted their interpretation of the “Negro Problem” from one defined by a deficient biological inheritance to one defined by a deficient culture.[5]
Health issues in segregated urban neighborhoods heavily populated by poor African Americans persisted throughout the twentieth century and into the Millennium. Many of the children raised in high-stress social and economic conditions experience—disproportionately when compared to children in higher-income neighborhoods—problems with vision, hearing, oral health, lead exposure, asthma, and obesity. Prenatal smoking and prenatal alcohol use, which occur disproportionately in poor neighborhoods, are often factors in premature births and low birth rates, the latter occurring among African American women at twice the rate as whites.[6]
[1] Kahlil Gibran Muhammad, The Condemnation of Blackness: Race, Crime and the Making of Modern America (Cambridge, MA: Harvard University Press, 2010), chap. 1.
[2] Ibid., chap. 2, quotes from p. 39.
[3] Ibid., 65, 67– 68, 70–73, 81.
[4] In 2012, Penn awarded Du Bois posthumously an honorary emeritus professorship. For an excellent narrative of Du Bois’s sojourn and enduring presence at Penn, see Greg Johnson, “The Times and Life of W.E.B. Du Bois at Penn,” Penn Today, 22 February, 2017; accessed from https://penntoday.upenn.edu/spotlights/web-dubois-penn.
[5] Muhammad, Condemnation of Blackness, chaps. 2, 3.
[6] Richard Rothstein, Class and Schools: Using Social, Economic, and Educational Reform to Close the Black-White Achievement Gap (Washington, DC: Economic Policy Institute, 2004), chap. 1. In 2014, Flint, Michigan, which is 57 percent African American with 45 percent of its residents living in poverty, provided a forceful example of government disregard of the health and sanitation needs of low-income urban communities. Flint experienced a catastrophic water contamination crisis when government officials, seeking to cut corners in city and state budgets, changed the City’s water supply from the Detroit River and Lake Huron to the Flint River—and failed to take adequate precautions to prevent aged pipes from leaching lead toxins into the drinking water. Consequently, as many as 12,000 children were exposed to levels of lead poisoning that may leave them permanently cognitively impaired. Regrettably, Flint followed a trend in the second half of the twentieth century of misguided public policies, government actions, and court rulings that had serious healthcare implications for poor African American communities. A case in point was the perpetual “drug crisis” of postwar urban America. Local, state, and federal governments regarded episodic epidemics of heroin and crack cocaine as the upshot of criminal acts committed by addicted users rather than as symptoms of widespread disease. Government’s response was punitive, replete with heavy-handed policing, no-excuses prosecution, and minimum mandatory sentences, which resulted in the mass incarceration of African American males beginning in the 1980s and continuing into the 2010s. Unlike the contemporary opioid crisis, which is largely a White phenomenon, heroin and crack addiction in poor African American neighborhoods was not viewed as an epidemiological problem that warranted counseling, treatment, and rehabilitation. Compounding this injury to health and human dignity, some municipal governments were guilty of locating toxic-waste-disposal sites and medical-waste incinerators in the poorest of these neighborhoods and tolerating illegal dumping. “Flint Water Crisis,” factual material accessed from https://en.wikipedia.org/wiki/Flint_water_crisis, 21 March, 2019; For the criminalized addiction-mass incarceration connection, see James Forman Jr., Locking Up Our Own: Crime and Punishment in Black America (New York: Farrar, Straus and Giroux, 2017); Michelle Alexander, The New Jim Crow: Mass Incarceration in the Age of Colorblindness, rev. ed. (New York: New Press, 2012). For state-sanctioned or -tolerated environmental abuses that afflict low-income African American children, see Richard Rothstein, The Color of Law: A Forgotten History of How Government Segregated America (New York: Liveright, 2017), 54-56; Jonathan Kozol, Savage Inequalities: Children in America’s Schools (New York: Crown, 1991), chap. 1; Jonathan Kozol, Amazing Grace: The Lives of Children and the Conscience of a Nation (New York: Crown, 1995), chap. 1.